Emergency Medical Services Systems. An overview.
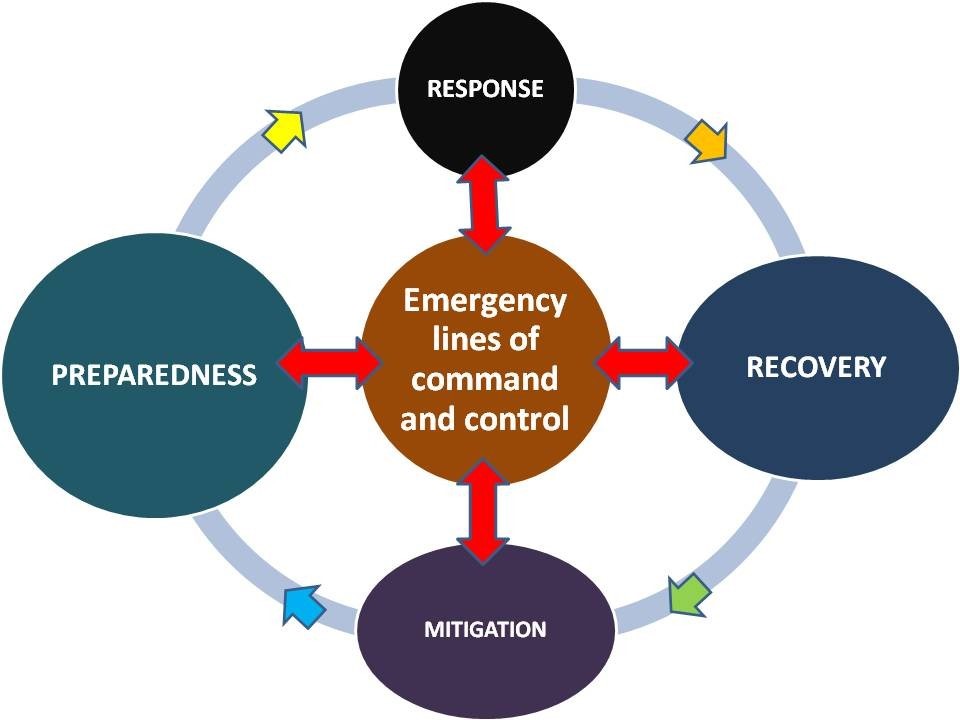
Emergency service protocols apply in an emergency. They usually start with planning before an emergency occurs, and require at least local explicit lines of command and control. Internationally recognized guidelines and networks are warranted; however, they are insufficiently active and effective nowadays.
The planning phase should guarantee preparedness, i.e. the set of guidelines suited for responding to a given incident, disease, trauma or set of circumstances. Due to the multiple agencies potentially involved, and called upon, lines of command and control must be clear and set in advance, allowing division of activities between agencies.
The response phase is a matter of integration of several plans, facilities and human resources committed to execute plans and tasks. Nonetheless, at the end the professionals may be called to improvise some areas of their response (due to gaps in the planning phase, which are inevitable due to the individual nature of most incidents). Personal expertise of human resources available is a key point in this regard.
Agencies may then be involved in recovery following the incident, where they assist in the clear up from the incident, or help the people involved overcome their mental trauma.
The final phase in the circle is mitigation, which involves taking steps to ensure no re-occurrence is possible, or putting additional plans in place to ensure less damage is done. This should feed back into the preparedness stage, with updated plans in place to deal with future emergencies, thus completing the circle.
This is not an all-purpose scheme, particularly when dealing with health services and facilities in which the coordination with progressively higher levels of medical specialization is necessary.
Clinical risk analysis and management
The most used approach in medicine, inside the hospitals and other care facilities is the Clinical risk analysis and management. It specifically is concerned with improving the quality and safety of health- care services by identifying the circumstances and opportunities that put patients at risk of harm and then acting to prevent or control those risks. This is the step closer to public health and health management. To expand the role of risk management across the organization, hospitals and other healthcare facilities are adopting a more holistic approach called Enterprise Risk Management. https://catalyst.nejm.org/what-is-risk-management-in-healthcare/.ERM includes traditional aspects of risk management including patient safety and medical liability, but also process analysis and out-hospital related services, and expands them with a “big picture” approach to risk across the organization. A macro-view can be adopted at national and supranational level, including the European Union.
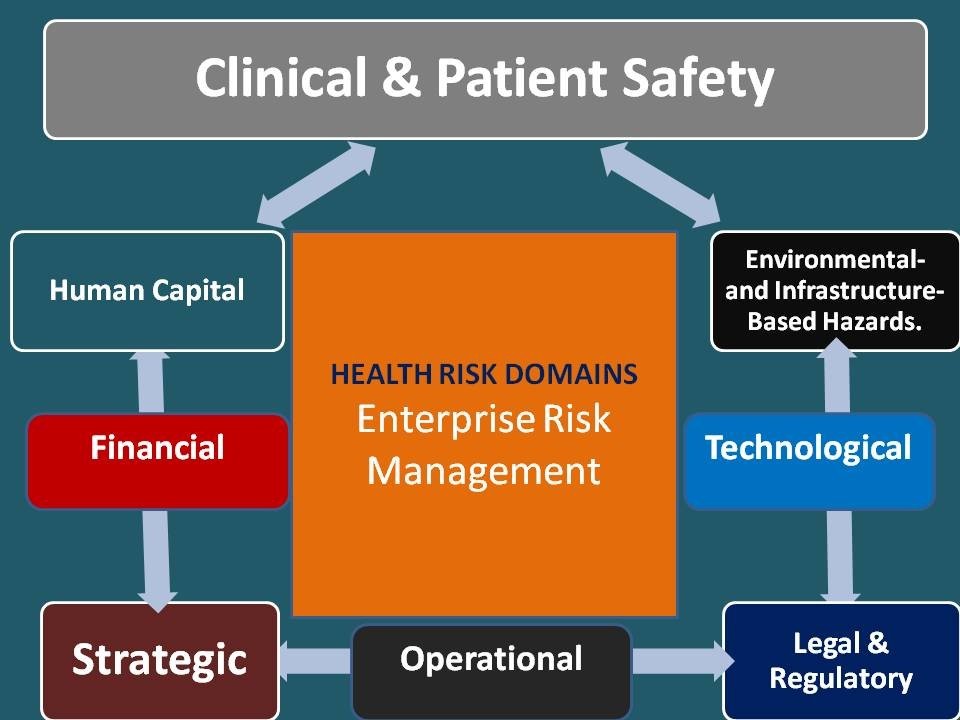
ERM encompasses eight risk domains:
- Operational;
- Clinical & Patient Safety;
- Strategic;
- Financial;
- Human Capital;
- Legal & Regulatory
- Technological;
- Environmental- and Infrastructure-Based Hazards.
The rapid response system
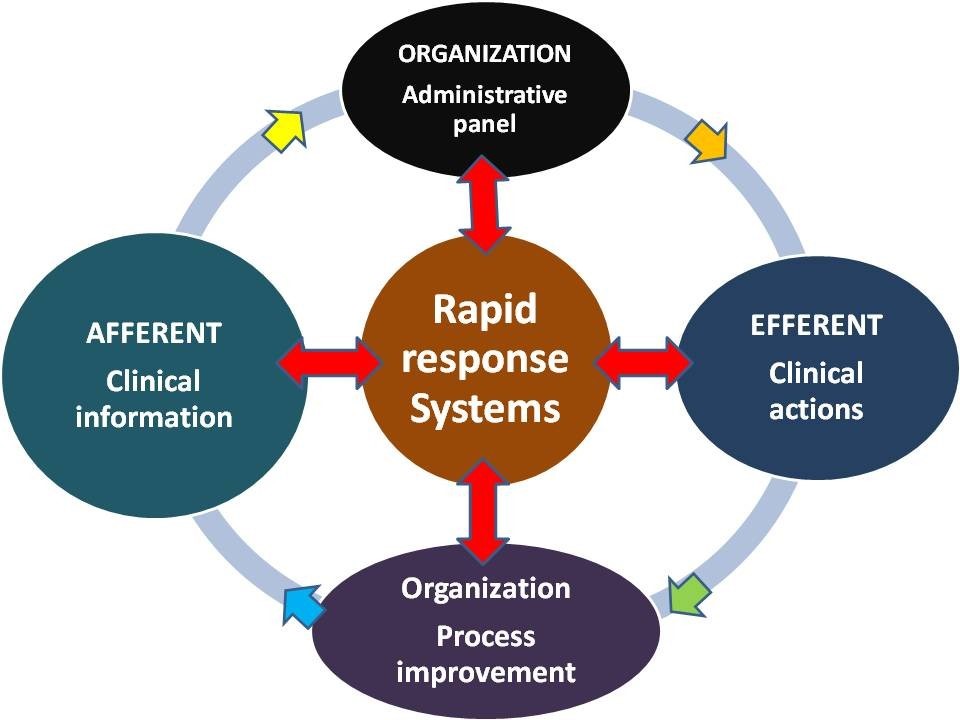
The rapid response system (RRS) is a strategy and a family of tools implemented in hospitals designed to identify and respond to patients with early signs of clinical deterioration on non-intensive care units with the goal of preventing respiratory or cardiac arrest, or other ominous events, such as stroke or renal-liver failure. A RRS consists of two clinical components (afferent and efferent) and two organizational components (process improvement and administrative).
All the above processes and concepts may be encompassed by the Reliability Engineering within the Medical Device and in any health system sector. Reliability is defined as the probability that an item, a process or a procedure, will perform a required function without failure under stated conditions for a specified period of time. Reliability Engineering increases the useful life of products, processes and services.
The above itemized approaches are mostly in use within modern hospitals, but its application is suitable also for ambulance intervention.
Strategies for innovation and development
The areas of expertise and intervention to be developed for allowing the organization of sustainable and reliable health emergency systems can be itemized in few points:
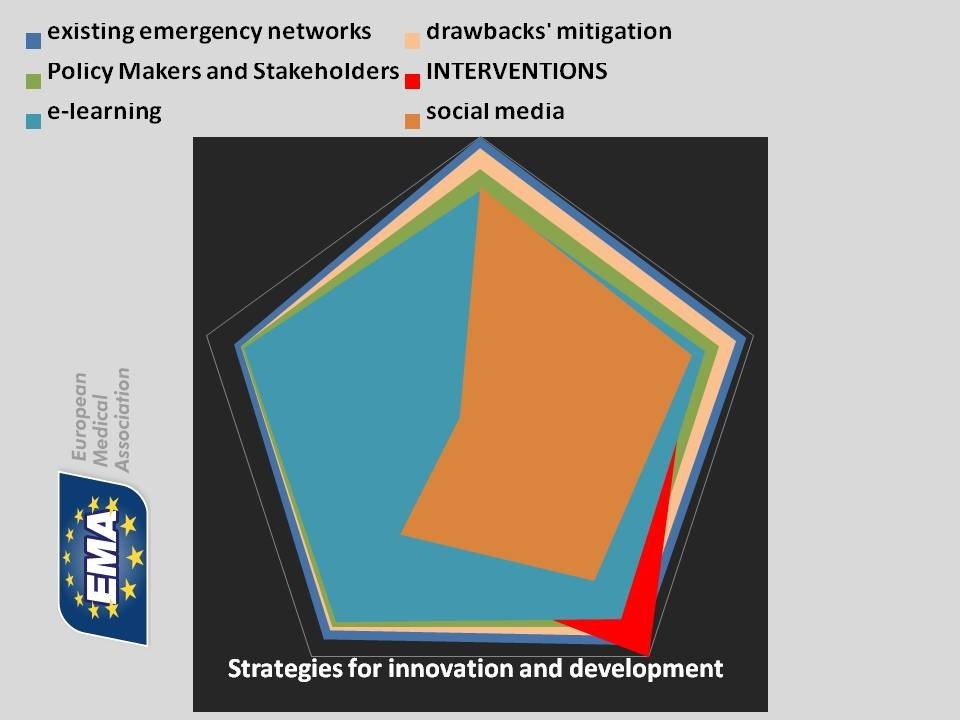
1) The analysis of the existing networks for facing emergencies, their level of complementarities, effective coordination, overlaps and even contradictions which can be detected, even occasionally.
2) Models of mitigation of these drawbacks, using simulation and, at large, bioinformatics when management of big data is necessary.
3) Proposals to Policy Makers and influential stakeholders, such as regional health managers, with timely implementation of pilot experiences.
4) Expert use of social media, particularly those web-based such as twitter and facebook, for dissemination of analysis, challenges, ideas, proposals toward both toward specialized and general audiences, displaying samples of meaningful scenarios.
5) Expert use of e-learning tools, to be used for teaching and training health professionals, and, in appropriate versions, to train other categories of users (schools, industries, other communities).
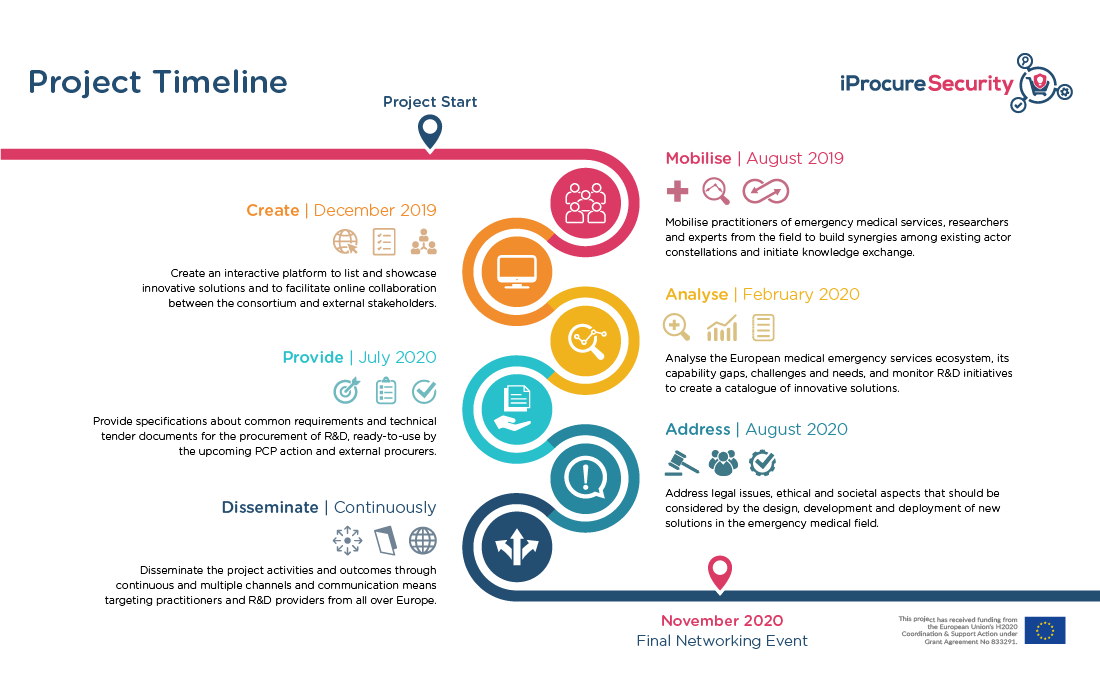
IProcure Security Project
The IProcure Security Project. Emergency Medical Services in Europe are characterized by a pluralistic landscape with diverse organizational setups, professional standards, coordination mechanisms and actors which result from different historical and institutional contexts in EU member states. However, diversity is united by the common aim, of providing timely care to victims of sudden and life-threatening injuries, emergencies or disasters in cross-border settings and international humanitarian missions.
Fostering the response capacities and increasing the cooperation of the European Emergency Medical Services Systems (EMSS) is of decisive importance for strengthening the resilience of European societies in the light of multiple hazards thus calling for close cooperation of public safety and health authorities on an international level.
iProcureSecurity seeks to identify the major challenges the system’s diversity poses to the capability of working together, stimulate R&I uptake with a view to increasing standardization of operations across Europe, and deliver technical requirements for R&I activities to prompt a more homogeneous European system of Medical Emergency Teams capable of working as one cohesive unit.
Acknowledgement: Prof. Guglielmo Trovato, MD, former professor of Internal Medicine and Director of the Postgraduate School of e-Learning in Health Sciences and Telemedicine of the University of Catania, Italy, provided suggestions and all the figures. The original drawings are included by his personal courtesy and were presented at the 2018 Congress of the European Medical Association, in the Lecture of the Acute and General Medicine Meeting, Excel, London 2018. I am indebted also with the many EMA Members working in the fields of Health Emergency whose lasting collaboration made possible this synthetic overview.
Disclaimer: The European Commission support for the iProcureSecurity does not constitute an endorsement of the contents of this article, which reflect the views only of the author, and the Commission cannot be held responsible for any use which may be made of the information contained therein.
Author: Vincenzo Costigliola, MD
Founder & President at European Medical Association (EMA)

